Women’s Sleep Disorders: Conquering Insomnia

Most women are familiar with lying awake at night gazing at the ceiling, hoping sleep will arrive. Insomnia, a pervasive sleep disorder, prevents falling asleep, sleeping, or feeling rested upon waking. It impacts daily functioning, causing women to feel tired and hazy throughout the day. In fact, one in four women deals with insomnia symptoms like trouble falling asleep or waking up too often. Women face this issue more than men—by about 40% over their lifetimes. This article explores the causes of insomnia in women, its signs, effects, and effective treatments for women with insomnia to help them find better rest.
Understanding Insomnia: Types and Prevalence
Insomnia is in two broad categories: short-term, lasting days or weeks due to stress or change, and long-term, which persists for months. Long-term insomnia tends to be associated with other medical conditions. Women indicate poorer sleep quality across all ages, taking longer to fall asleep and being more sleepy during the day. Older women have even greater risks, with hormonal factors on women’s insomnia being a significant influence.
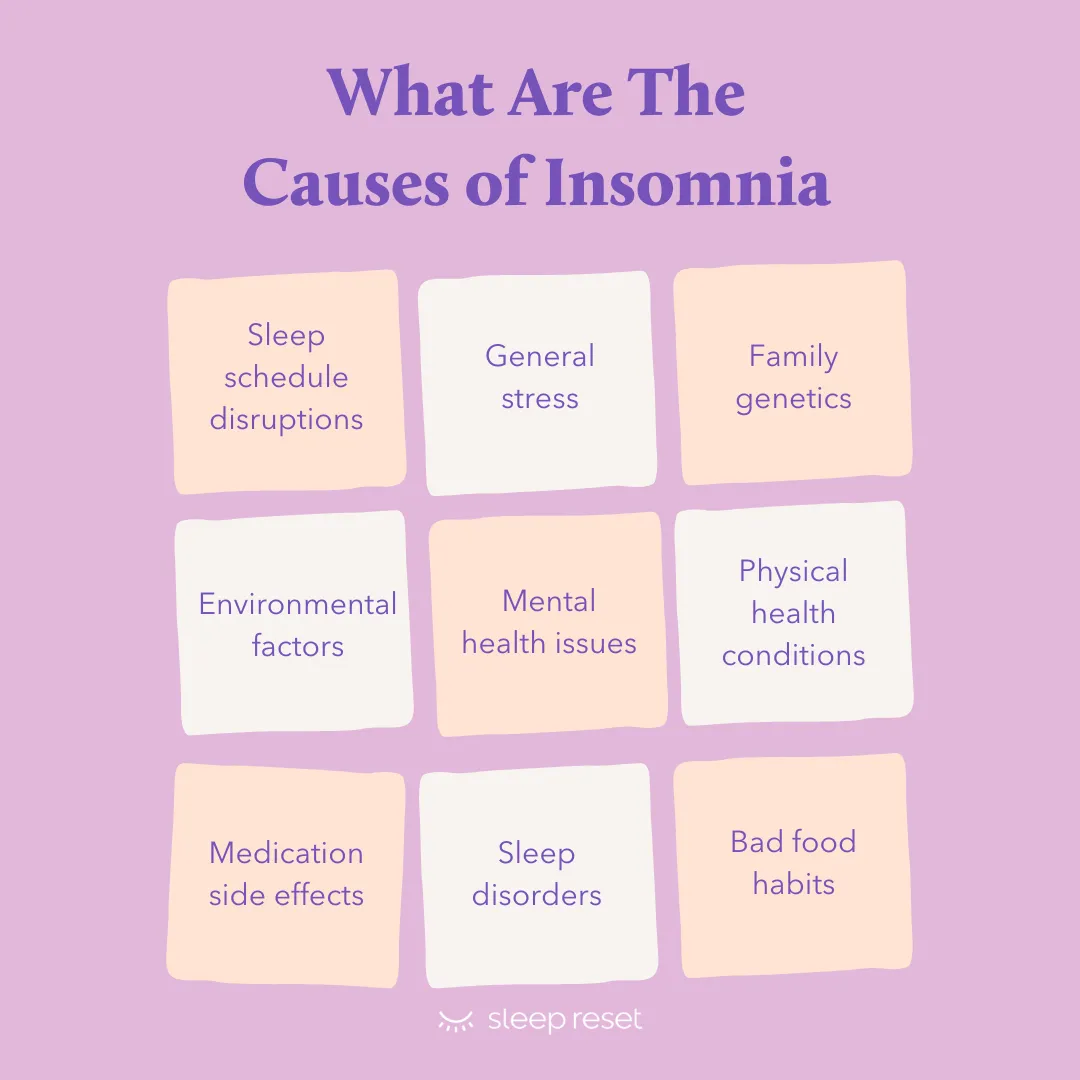
Causes of Insomnia in Women
Also Read: Mental Self-Care Activities To Reduce Stress
So, why is insomnia so prevalent in women? The etiology of insomnia in women is biology and the demands of life. The hormones are at the forefront. Throughout the menstrual cycle, particularly the fourteen days leading up to a period, the estrogen and progesterone levels change. These hormonal effects on women’s insomnia slice deep sleep and trigger arousals. Women with premenstrual syndrome (PMS) or severe premenstrual dysphoric disorder (PMDD) experience added pain, mood swings, and poorer response to melatonin, the sleep hormone. Cramps or heavy bleeding rob others of sleep throughout the night.
Insomnia During Pregnancy
Pregnancy cranks it up. During the initial months, exhaustion is severe, but by the third trimester, discomfort is in charge. Backache, heartburn, constant trips to the bathroom, and kicks from baby disturb sleep. Restless legs syndrome (RLS), which strikes as many as 20% of pregnant women, brings twitching and discomfort, joining the causes of insomnia for women. After giving birth, new mothers fight changing hormones, baby feedings, and anxiety, with insomnia persisting for months. Less than six hours of sleep increases depression risk in these periods.
Menopause and Insomnia
Menopause also brings its own whirlwind. Perimenopause, the transitional phase, witnesses hot flashes and night sweats in nearly all women, startling them in the middle of the night. Follicle-stimulating hormone increases, breaking up sleep, while low estrogen is associated with difficulty maintaining sleep. These hormonal effects on women’s insomnia result in as many as 42% of women at this stage suffering from chronic insomnia. Sleep apnea, previously considered largely a man’s problem, spikes after menopause, commonly confused with plain insomnia.
Stress, Mood, and Lifestyle Factors
Beyond hormones, mood and stress are big. Women lose more sleep worrying—about work, family, or health. Depression and anxiety hit women twice as frequently as men, and fuel insomnia in a vicious cycle. Insomniacs are 10 times more likely to be depressed and 17 times more likely to be anxious. Pain that’s chronic, such as migraines, fibromyalgia, or arthritis—more prevalent in women—keeps bodies on high alert. Caregiving responsibilities, from children to seniors, push bedtimes late, conflicting with women’s earlier intrinsic sleep clocks, contributing to the etiologies of insomnia in women.
Lifestyle habits creep in as well. Working the night shift, traveling, or a snoring partner disrupt rhythms. Caffeine, alcohol, or screens at bedtime make matters worse. Even hormone therapy for trans women can awaken sleep disturbances, such as hot flashes or pauses in breathing. Racial and ethnic minority women, and LGBTQ+ individuals, have additional obstacles through discrimination and access barriers, increasing rates of insomnia.
Symptoms and Effects of Insomnia
Symptoms of insomnia appear at midnight and noon. At nighttime, a woman may lie awake for more than 30 minutes to fall asleep, wake repeatedly, or get up too early, unable to fall back to sleep. She doesn’t feel rested despite hours in bed. During the day, fatigue lingers—low energy, crankiness, or difficulty concentrating. Memory lapses, moods fluctuate, and activities such as driving become hazardous. Close to one-third of women report insomnia causes impairment in daily life, more than men.
Health Impacts of Insomnia
The cost runs deeper. Bad sleep is associated with weight gain, heart issues, compromised immunity, and increased accident risks. Psychologically, it increases anxiety, depression, and even suicidal thoughts. In pregnancy, poor sleep increases risks of preterm delivery or diabetes. During menopause, it exacerbates hot flashes and mood swings. Over time, insomnia women have increased fibromyalgia or respiratory disorders. However, many quietly endure, believing it’s “just life.”
How to Improve Women’s Sleep Quality
To combat insomnia, begin with knowing it is a treatable condition. Begin with eliminating the reasons why women get insomnia—a physician tests for thyroid, pain, or medication side effects. Keep a sleep diary to monitor patterns: bedtime, wake-up time, caffeine consumption. Improving women’s sleep begins with these actions.
Lifestyle Adjustments
Lifestyle adjustments constitute the foundation of treatments for insomnia in women. Maintain a regular sleep schedule, even on weekends—seven to nine hours of sleep. Wind down with no screens an hour prior to bedtime; their blue light suppresses melatonin. Dim lights, book, or warm baths. Make the bedroom cool, dark, and quiet—earplugs or fans. Exercise every day, but not close to bedtime. Cut back on caffeine after noon and alcohol nights; heavy dinners close to bedtime churn the gut. These are the secrets to improving women’s sleep quality.
Relaxation Techniques
Relaxation aids calm the mind. Deep breathing, meditation software, or soothing yoga at bedtime soothe frenzied thoughts. Writing down troubles on paper jettisons anxieties. For RLS during pregnancy, stretches of light or iron tests are wonders of care as part of successful treatments for pregnant women with insomnia.
Effective Treatments for Women with Insomnia
Also Read: How Is AI Helping With Mental Health Solutions For Women
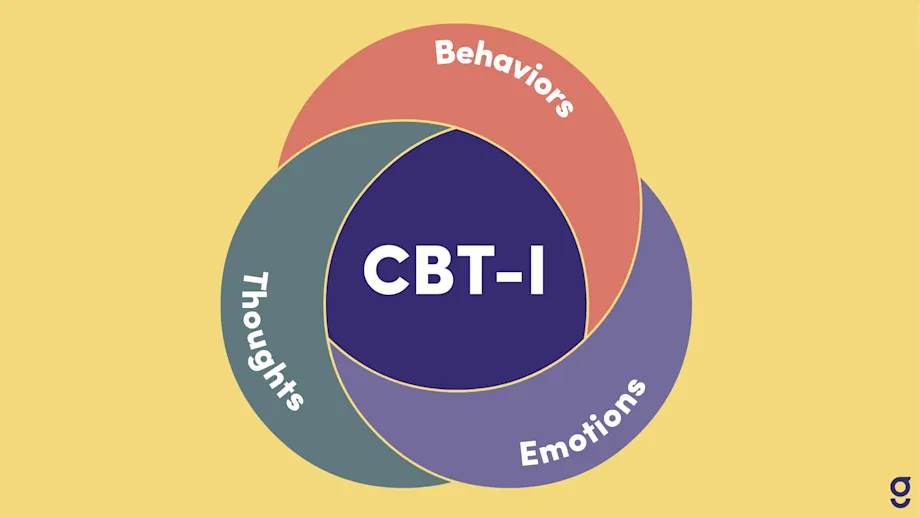
Cognitive Behavioral Therapy for Insomnia (CBT-I)
If fundamentals don’t work, cognitive behavioral therapy for insomnia (CBT-I) is a star. This therapy talk, usually six to eight sessions, reprograms sleep thinking—such as replacing “I’ll never sleep” with soothing plans. It rivals meds in effectiveness but has longer duration, without drowsiness. Apps provide digital CBT-I, convenient for busy women. It reduces symptoms in menopause, too, so it’s a leading contender among successful treatments for women insomniacs.
Medications and Supplements
Meds are next, short-term. Over-the-counter antihistamines such as diphenhydramine help some, but briefly. Prescription medications are “Z-drugs” such as zolpidem (smaller doses for women, since bodies work more slowly) or newer ones such as daridorexant. Antidepressants such as trazodone also help mood and sleep. Melatonin supplements are appropriate for jet lag or shifts, but consult physicians—quality is variable. For menopause, hormone therapy makes hot flashes disappear, improving sleep in some, although outcomes are mixed. These medical options are part of effective treatments for women with insomnia.
Alternative Therapies
Alternative aids like acupuncture or yoga show promise, especially for perimenopause. A Mediterranean diet—fruits, veggies, fish—cuts sleep woes in older women, paired with less booze and caffeine. If pain or apnea lurks, treat those first. These approaches also contribute to how to improve women’s sleep quality.
Conclusion
Women are entitled to sound nights. Insomnia robs energy, but tiny adjustments and care win it back. Consult a physician if nights stretch out three weeks—early intervention avoids grip that becomes chronic. With time, many women wake up refreshed, prepared for better days.