Thyroid Health In Women: How Hormonal Changes Impact The Gland

The thyroid gland quietly conducts much of the body’s daily rhythm, sitting in the neck like a small butterfly-shaped boss. It produces hormones that maintain energy levels steady, help in weight management, and even affect mood. This gland has to deal with more stressors in women because of the natural ups and downs of the body’s hormones. From the first signs of puberty to the shifts of menopause, these changes can throw the thyroid off balance, leading to issues that impact daily life. Thyroid health is crucial here, wherein thyroid problems strike up to eight times more often in women than in men, especially during key life stages. Understanding how hormonal changes affect the thyroid in women helps women recognize warning signs early and enables them to take healthy steps.
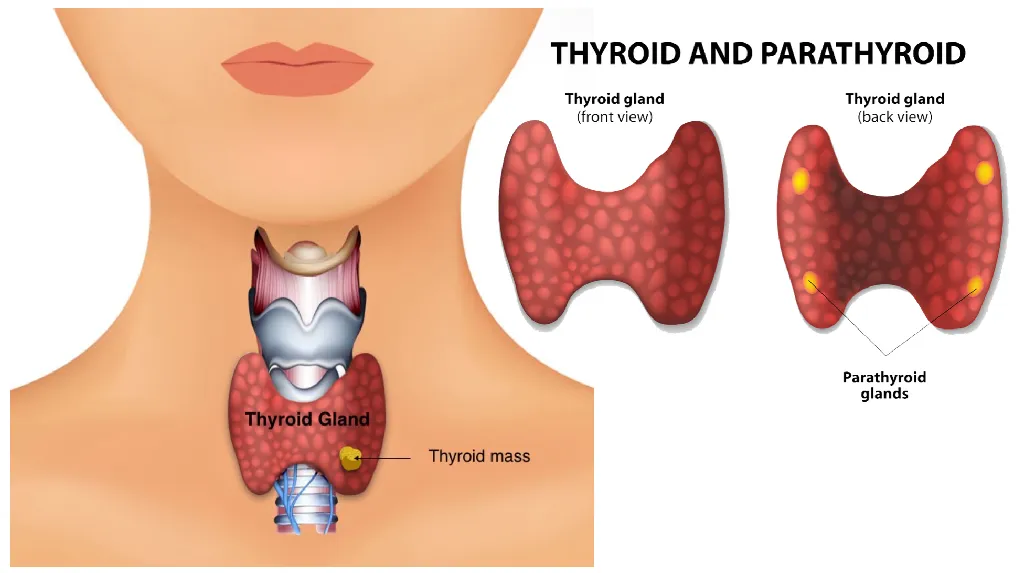
Overview of How the Thyroid Works
On a basic level, the thyroid manufactures two primary hormones: thyroxine, more commonly known as T4, and triiodothyronine, or T3. Both travel via the blood to organs everywhere, instructing cells to accelerate or decelerate. They play a big role in metabolism—the way the body turns food into fuel. A healthy thyroid keeps heart rate even, bones strong, and skin glowing. But if something disrupts it, things can go haywire.
The pituitary gland in the brain acts like a referee, sending signals through TSH to tell the thyroid what to do. Iodine from food is key, too, because it’s a critical building block for those hormones. Women’s bodies, tuned to cycles of estrogen and progesterone, can often pull on this system in unique ways. Estrogen, for example, can ramp up the proteins that ferry thyroid hormones, which means the body might need more to keep levels right. It’s a delicate dance, and hormonal shifts can step on toes.
Key Hormonal Changes and Their Connection to the Thyroid
Also Read: Women’s Sleep Disorders: Conquering Insomnia
Women’s lives are a succession of waves of hormone changes, each rippling through the thyroid in its own particular way. Let’s break them down.
Puberty and the Menstrual Cycle
Puberty starts with a rise in estrogen, which puts the thyroid on an increased work order to support growth spurts and budding fertility. This increased demand is generally well tolerated but establishes the stage for sensitivity. As the cycles settle in, the monthly ebbs and flows of estrogen and progesterone keep the thyroid on its toes. Even slight adjustments in thyroid levels can shorten or lengthen periods or make them heavier. For some, this translates into subtle imbalances that build over time.
Pregnancy: A Period of Increased Needs
Pregnancy is a thyroid marathon. Human chorionic gonadotropin, the hormone behind morning sickness, mimics TSH and boosts thyroid output early on. Estrogen levels skyrocket, doubling or tripling the need for thyroid hormones to support the growing baby. Pregnancy and thyroid hormone levels become critical here. Until its own thyroid starts at around 12 weeks, the fetus depends on mom’s supply. If mom’s thyroid doesn’t keep pace, the risk for miscarriage, preterm birth, or developmental issues in the child rises. Up to 10% of pregnancies involve thyroid glitches, often hypothyroidism. Postpartum hormone drops can trigger flare-ups, like in Hashimoto’s thyroiditis, an autoimmune attack on the gland.
PCOS and Other Fertility Hurdles
Polycystic ovary syndrome really muddies the waters. With PCOS, high androgen and insulin resistance often come hand in hand with thyroid woes to create an inflammatory cycle. Women with PCOS run a higher risk of hypothyroidism, further worsening irregular periods and weight struggles, as if the hormones are in a yelling match and the thyroid gets caught in the crossfire.
Menopause: The Estrogen Fade-Out
As women approach menopause, usually in their 40s or 50s, estrogen dips sharply. This slowdown reduces the thyroid’s workload but also makes it less efficient. Iodine uptake drops, and free T3 and T4 levels may fall, nudging toward hypothyroidism. Thyroid problems during menopause symptoms like hot flashes, fatigue, and mood swings from menopause often mimic or mask thyroid symptoms. Postmenopause, risks climb for nodules, goiters, and even thyroid cancer—the highest rates hit older women. Bone loss and heart issues from low thyroid function add to the toll, especially since estrogen once protected those areas.
And these changes do not happen in isolation. Stress, poor diet, or genetics can amplify them, causing minor wobbles to become full disorders.
Thyroid Issues Due to Hormones

Also Read: Mental Self-Care Activities To Reduce Stress
When hormones disturb the thyroid, it gives way to two major problems: underactivity, known as hypothyroidism, and overactivity, known as hyperthyroidism.
Hypothyroidism is the sneaky one, slowing everything down. That comes from Hashimoto’s: a condition where your immune system attacks the thyroid, often during pregnancy or perimenopause. Low thyroid hormones tank estrogen and testosterone, too, making a mess of cycles and libido. Like in Graves’ disease, hyperthyroidism revs things with excess hormones-a problem sometimes triggered by surges of estrogen. Less common, but hit hard with rapid heartbeats and anxiety that echoes hormonal chaos.
Both can be based on autoimmune etiology, which peaks in women because of the immuno-enhancing effects of estrogen. In peri- and postmenopausal phases of life, thyroid glitches add to the risks of heart disease and osteoporosis.
Symptoms Overlap: How to Recognize the Signs
Most thyroid issues in women mask themselves behind hormonal symptoms. Fatigue that lingers? It could be low thyroid or perimenopause. Unexplained weight gain or loss? Thyroid imbalance or estrogen flux. Dry skin, thinning hair, or brittle nails scream hypothyroidism, while heat intolerance and shaky hands point to hyperthyroidism.
Mood dips, such as irritability or brain fog, blur lines with PMS or menopause blues. Other symptoms include irregular periods, infertility, or heavy bleeding, which may ring an alarm of thyroid dips affecting reproductive hormones. Constipation or swelling during pregnancy may be subtle signs that get blamed on “normal” changes. Listening to the body—tracking patterns over months—helps separate the threads.
Diagnosis, Treatment, and Everyday Care: Step by Step
It all starts with catching it early-a visit to see the doctor. Blood tests for TSH, free T4, and antibodies paint a picture. Ultrasound spots the nodules, and sometimes fine-needle biopsies check for cancer.
The treatment is simple: synthetic hormones, namely levothyroxine, cure hypothyroidism, which one has to take daily for their whole life. For hyperthyroidism, medications, radioactive iodine, or surgery calm the overdrive. In menopause, hormone therapy might sometimes help ease the overlying symptoms, but doctors are very cautious with that treatment.
Lifestyle can help. A balanced diet of seafood, nuts, and veggies rich in iodine helps the gland; 150 micrograms per day will do, but avoid too many supplements. The metabolic rates improve with exercises like brisk walking without putting undue pressure on the body. Stress busters, like yoga or a sleep routine, put a check on cortisol from further stressing the thyroid. Natural ways to support thyroid during hormonal changes include these habits. Regular check-ups are very beneficial for women in hormonal flux, mainly if family history is lurking.
Wrapping It Up: Empowering Thyroid Wellness
The hormonal changes that shape thyroid health in women, from vibrant puberty to wise menopause, require attention, not fear. Awareness turns potential pitfalls into manageable paths. By tuning into symptoms and in league with healthcare pros, women can nurture their thyroid health through each phase. A strong, healthy gland means more energy for living fully. Thyroid health is essential throughout all stages of life.