Medical Misogyny, Late Diagnoses, Social Determinants, And Health Gaps By Race, Income, And Geography.

Healthcare systems around the world are meant to benefit everyone, but they frequently fail to do so for some groups of people. Women, members of racial minorities, people with low incomes, and people living in rural areas face huge problems. These include medical misogyny, which is a type of sexism in the medical field, resulting in late or missed diagnoses. Social determinants such as education, housing, and social support are also involved. Health inequities increase based on race, income, and geography. Health inequities impact many people every day. This article examines these problems in depth, using simple language to illustrate how they are all interrelated and impact people’s lives. Health inequities require attention today. Health inequities by race and income impact women most. Health inequities persist in all geographic areas. Health inequities continue to increase unchecked.
Understanding Medical Misogyny in Healthcare
Medical misogyny is the term used to describe the long-standing bias against women in the healthcare system. It originated from the long-held belief that women’s bodies and complaints are less significant or more difficult to grasp than men’s. For decades, medical studies focused mostly on men, assuming results applied to women. As a result, treatments and diagnoses often ignore how diseases affect women differently. In one common case, heart disease in women gets overlooked because symptoms like fatigue or jaw pain do not match the “classic” male signs, such as chest pain. This is sometimes called Yentl syndrome, where women must mimic male symptoms to get proper care.

Also Read: How Women Live Longer, Despite Being In Poor Health Compared To Men
How Gender Bias Leads to Missed Diagnoses in Healthcare
Gender bias leading to missed diagnoses in healthcare is a serious problem. Women wait longer for answers on conditions like endometriosis, a painful disorder affecting the reproductive system. On average, it takes seven to ten years for a diagnosis because symptoms like heavy periods or cramps get brushed off as normal. Autoimmune diseases, which hit women more often, also face delays. Lupus or multiple sclerosis might be labeled as anxiety or depression first. In cancer care, breast and ovarian cancers link to gender inequality worldwide, with higher death rates in places where women have less power. These delays mean worse outcomes, more suffering, and higher costs for treatment later on.
The Role of Social Determinants of Health in Inequities
Social determinants of health add another layer to these inequities. These are the non-medical factors that shape well-being, such as where people live, their jobs, education, and support networks. For women, these often intersect with gender roles. Many women juggle work, childcare, and elder care, leaving less time for doctor visits. Poor housing or unsafe neighborhoods can increase stress, leading to health issues like high blood pressure. Access to healthy food and clean water also matters. In low-resource areas, these basics are hard to get, worsening conditions like diabetes or heart problems.
Health Gaps by Race and How Bias Compounds

Also Read: The Persistent Burden Of STIs (HIV, HPV, Syphilis, Chlamydia) On Young Women
Health gaps by race highlight how bias compounds. Black women in the United States, for instance, die from pregnancy-related causes at three to four times the rate of white women. This stems from racism in healthcare, where providers might ignore their concerns or provide lower-quality care. Studies show that racial minorities face longer wait times and fewer referrals to specialists. Indigenous and Hispanic women also deal with language barriers and cultural misunderstandings, leading to missed screenings for cancers or chronic diseases. In global terms, women in regions with high gender inequality see more cervical and breast cancer deaths due to limited screening and treatment.
Income Disparities and Their Impact on Healthcare Access
Income plays a huge role in these disparities. Low-income families struggle with healthcare costs, even in countries with public systems. Women, who often earn less than men, might skip check-ups or medications to save money. This leads to untreated conditions like hypertension or mental health issues. In the U.S., uninsured rates are higher among low-wage workers, many of whom are women of color. Globally, poverty limits access to birth control or prenatal care, raising risks for mothers and babies. Wealthier people can afford private care or travel for specialists, widening the gap.
Geographic Barriers and Rural vs Urban Challenges
Geography creates barriers too. Rural areas often lack hospitals, specialists, or even basic clinics. Women in remote places might drive hours for a mammogram or obstetric care, delaying treatment. Urban poor face different issues, like overcrowded facilities or pollution-related health problems. In developing countries, geography ties to income and race, with indigenous groups in isolated areas getting the least resources. Climate change adds to this, as floods or droughts hit rural health harder, affecting food security and disease spread.
Also Read: Contraception: Global Access And The Unmet Need Of Millions Of Women
Intersectional Overlaps: Multiple Layers of Bias
These factors do not exist alone; they overlap in intersectional ways. A low-income Black woman in a rural area faces triple bias: racism, sexism, and classism. For example, during the COVID-19 pandemic, these groups had higher infection and death rates due to jobs in essential services and poor access to vaccines. Transgender and non-binary people experience even more layers, with gender bias mixing with discrimination against their identities.
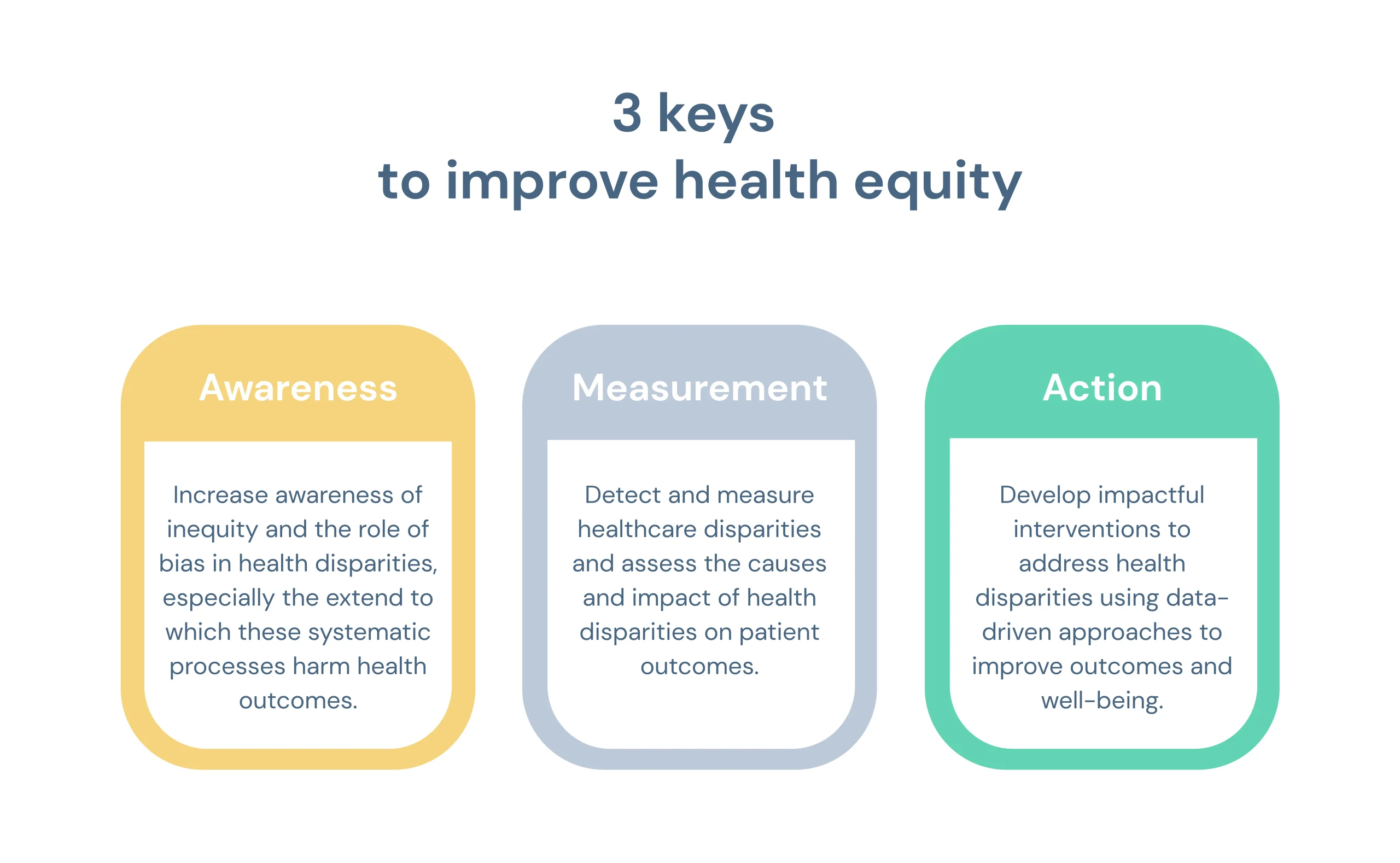
Growing Efforts to Address Healthcare Inequities
Efforts to fix these issues are growing. Training programs teach doctors about implicit bias, helping them listen better to diverse patients. Policies push for more women and minorities in medical research and leadership. Telemedicine helps bridge geographic gaps, allowing remote consultations. Community health workers, often from affected groups, build trust and improve access. Advocacy groups call for funding women’s health studies and addressing social determinants like affordable housing.
Why Closing These Gaps Matters for Everyone
In the end, healthcare inequities hurt society as a whole. Gender bias in healthcare access and treatment remains widespread. Racial and geographic disparities in women’s health continue to cause harm. Women’s health inequities by race and income create lasting damage. Closing these gaps means healthier families, stronger economies, and fairer systems. Progress requires listening to those affected and making changes at every level, from doctor offices to government policies. With ongoing work, a more equal healthcare future is possible.