The Invisible Women’s Health Gap: Understanding Endometriosis, PMS, Menopause, And Migraine
Women everywhere are facing a silent crisis that is grossly understated within healthcare systems worldwide. Millions of women worldwide suffer from invisible health issues such as endometriosis, PMS, menopause, and migraines-yet these conditions often go dismissed, underdiagnosed, or misunderstood. There are devastating consequences to this invisible women’s health gap: endometriosis PMS has serious consequences on women’s careers, relationships, and their overall quality of life.
What Is the Women’s Health Gap?
The women’s health gap describes the huge differences in awareness, research, and treatment of women’s health issues compared to those affecting men. For years, the majority of medical studies were based on men’s bodies, so women’s different invisible illnesses were inadequately researched and poorly documented. Nowadays, women suffer from pain and symptoms which are sometimes belittled or denied by healthcare providers, leading to delayed diagnosis and additional suffering.
This is more than a medical gap; it translates into very real economic and social consequences. Studies have shown that these invisible health problems cost women their jobs, financial security, and well-being.
Endometriosis: The 10-Year Diagnosis Gap
Endometriosis is a condition where tissue similar to the uterine lining grows outside the uterus, causing severe pain and fertility problems. Despite affecting approximately 180 million women worldwide, many women wait nearly a decade before receiving a proper diagnosis. Underdiagnosed migraines and endometriosis women face these invisible health issues daily.
Women with endometriosis often report excruciating pain during menstruation and sexual intercourse. Yet many healthcare providers dismiss their symptoms as “normal period pain” or suggest they are being overly dramatic. Young women especially struggle to be taken seriously, with some experiencing years of misdiagnosis or being told the pain is psychological.
The consequences are significant. Women miss work, school, and important life events. Some are forced to leave their jobs entirely. The emotional toll of not being believed compounds the physical suffering, leading to anxiety and depression in many cases.
PMS: Beyond the Stereotype
Also Read: Cycle Syncing And Holistic Living: Lifestyle Practices In Line with Hormonal Patterns In Women
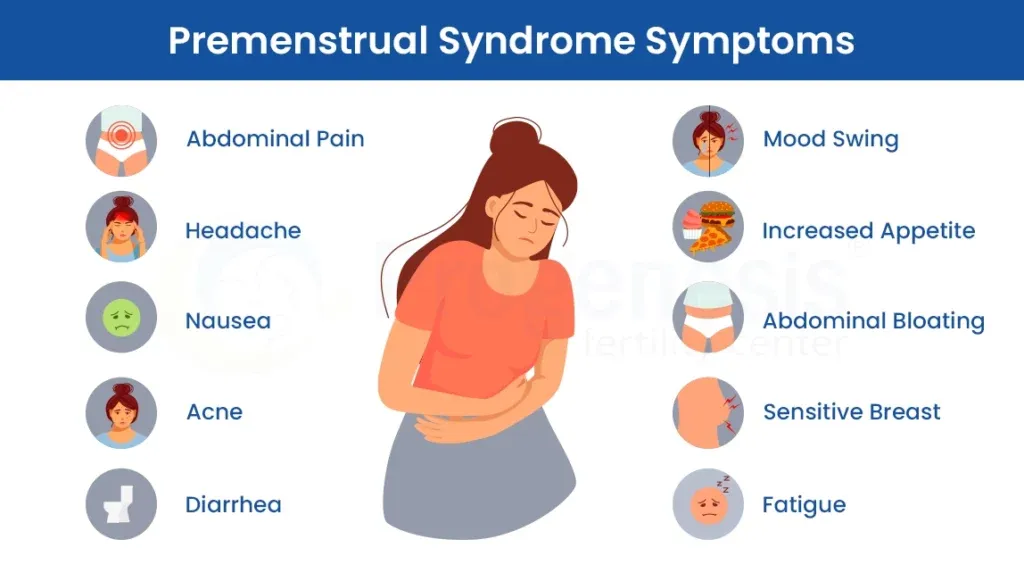
Premenstrual syndrome affects millions of women each month, causing physical and emotional symptoms that can be severely disabling. These symptoms include bloating, fatigue, mood changes, and severe cramping. However, PMS remains widely stereotyped and dismissed as women being “moody” or “overreacting.” The migraine PMS connection in women’s health makes these invisible health issues even more challenging.
The reality is far more serious. Severe PMS, known as premenstrual dysphoric disorder (PMDD), can be so debilitating that women cannot function at work or in their relationships during certain weeks of the month. Women lose productivity, miss important meetings, and may even experience relationship strain due to symptom severity.
Despite its widespread impact, PMS receives minimal research funding compared to other conditions. Effective treatments exist, but many women never learn about them because their symptoms are never taken seriously. The invisibility of PMS means that women silently struggle month after month, sometimes for decades.
Menopause: A Life Stage Dismissed as “Normal”
Menopause marks the end of a woman’s reproductive years, typically occurring in her late 40s or 50s. While it is a natural life stage, the symptoms women experience during menopause can be profoundly disruptive. Underresearched menopause and productivity loss highlight these critical invisible health issues.
Hot flashes, night sweats, sleep disruption, mood changes, and brain fog are common menopause symptoms that can last for years. Many women report that these symptoms significantly impact their work performance and personal relationships. Some are forced to reduce their working hours or take early retirement.
Yet menopause is often treated as an insignificant phase rather than a legitimate health concern. Women are sometimes told to “just deal with it” or that their symptoms are not real. This dismissal means that many women suffer in silence without seeking or receiving proper support and treatment.
The economic impact is substantial. When women leave the workforce due to menopause symptoms, companies lose experienced workers and women lose income and career progression opportunities.
Migraines: A Pain Condition Underestimated

Also Read: Abortion Restrictions And Their Impact On Women’s Health Systems Worldwide
Migraines affect women at nearly three times the rate they affect men, yet this condition remains significantly underfunded in research and often trivialized in public perception. Women with severe migraines experience debilitating pain, nausea, and sensitivity to light and sound that can last for hours or even days. Underdiagnosed migraines and endometriosis women suffer from these overlapping invisible health issues.
For many women, migraines are connected to their menstrual cycle, making them predictable but no less disruptive. The migraine PMS connection in women’s health creates predictable patterns of suffering. Women miss work, cancel social plans, and experience reduced quality of life due to the frequency and severity of their migraines.
Despite this significant gender difference, migraine research has historically focused more on men’s experiences. Treatment options for women remain limited, and women’s migraine symptoms are sometimes attributed to stress or anxiety rather than recognized as a legitimate neurological condition.
Why Does This Gap Exist?
Several factors contribute to the invisible women’s health gap endometriosis PMS:
- Historical Research Bias: Medical research has historically excluded women or used male-dominated samples, leaving women’s invisible health issues understudied.
- Symptom Dismissal: Women’s reported symptoms are often dismissed as emotional or exaggerated, leading healthcare providers to underestimate condition severity.
- Lack of Awareness: Both women and healthcare providers often lack awareness about these invisible health issues, their symptoms, and available treatments.
- Limited Funding: Research funding for women-specific health conditions remains significantly lower than funding for other health areas.
- Workplace Culture: Stigma around discussing these invisible health issues at work means many women suffer silently rather than seeking help or accommodations.
The Real-World Impact
The consequences of this invisible women’s health gap endometriosis PMS extend far beyond physical symptoms. Women lose income, miss career advancement opportunities, and experience damaged relationships due to misunderstanding and lack of support. Students miss classes and fall behind academically. Professional women reduce their working hours or leave careers entirely. Underresearched menopause and productivity loss shows the true scale of these invisible health issues.
Additionally, the emotional toll of not being believed or having symptoms dismissed can lead to anxiety, depression, and a sense of isolation. Women internalize the message that their suffering is not legitimate, which compounds their distress.
Moving Toward Solutions
Closing the invisible women’s health gap endometriosis PMS requires action at multiple levels. Healthcare providers need better training to recognize and take women’s invisible health issues seriously. Medical schools must emphasize women’s health research and ensure that women are adequately represented in clinical trials.
Research funding must be redirected toward understanding these conditions better, particularly addressing underresearched menopause and productivity loss. Policy makers can support this by mandating gender-balanced research and increasing funding for women’s health studies.
Workplace policies need to evolve to support women experiencing these invisible health issues. Flexible work arrangements, remote work options, and open conversations about health can help women manage their conditions while maintaining their careers.
Finally, cultural change is essential. Society must move away from dismissing women’s health concerns and recognize these conditions as legitimate, serious health issues that deserve attention and compassion.
Conclusion
The invisible women’s health gap endometriosis PMS represents a significant failure of healthcare systems to adequately serve half the population. Endometriosis, PMS, menopause, and migraines are not minor complaints—they are serious health conditions that dramatically impact women’s lives. By acknowledging this gap, investing in research, training healthcare providers, and supporting workplace changes, society can begin to close this gap and ensure that women receive the care, understanding, and support they deserve.









